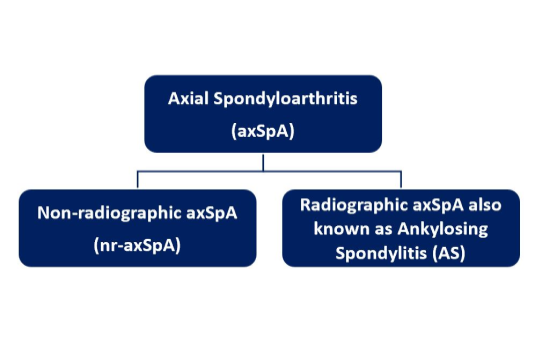
What is Axial Spondyloarthritis and Ankylosing Spondylitis?
Axial spondyloarthritis (axSpA) is an umbrella term for non-radiographic axSpA (nr-axSpA) and radiographic axSpA, also known as Ankylosing Spondylitis (AS). nr-axSpA and AS are closely related rheumatic conditions, both forms of inflammatory arthritis.
Inflammation is a normal part of the immune system, where blood flow is increased and specialised cells are sent to specific areas. While inflammation is usually an important part of the body’s defense against infection, it can become over-active, leading to conditions such as axSpA.
axSpA causes several parts of the lower spine to become inflamed, including the bones in the spine (vertebrae), spinal joints (sacroiliac joints) and other areas of the body. Over time, this can damage the spine and lead to the growth of new bone, which in some cases can cause parts of the spine to join up (fuse) and lose flexibility. This is known as ankylosis.
For people with AS, changes to the sacroiliac joints or spine can be seen on x-ray scans. However, for people with nr-axSpA these changes are not visible on x-ray, but inflammation may be visible on MRI (magnetic resonance imaging).